CUTTER BUSINESS TECHNOLOGY JOURNAL VOL. 32, NO. 4

Michael Gleeson discusses how public health agencies and emergency managers can leverage the digitization of contact tracing of airline passengers at risk from a biological outbreak. He outlines the increased risk of infection and spread, facilitated by the increased numbers of airline passengers globally. A global framework to prepare for and respond to a biological threat, natural or otherwise, spread via air travel, can be achieved through the digitization of contact tracing using a collaborative approach among the airline industry, public health agencies, and EM practitioners. Identifying and locating at-risk passengers in a fast and efficient manner is paramount to limiting contagion spread.
With the ever-increasing reach and speed of the global aviation network, contagion can spread anywhere in the world within 24 hours. As a result, the potential risk of introducing and spreading infectious disease is on the rise. This article explores the digitization of contact tracing of at-risk airline passengers in the event of a biological threat. With more than 4 billion airline passengers in 2017 and over 7 billion expected by 2036,1 the possible transmission in flight of infectious diseases is of the utmost concern to global health authorities. In fact, in 2003, the emergence of severe acute respiratory syndrome (SARS) showed the potential of a contagion to emerge, spread, and affect the health and social and economic life of people across the world.2
The Air Travel Reality
People’s increased mobility, facilitated by air travel, has resulted in the increased spread of contagion across geopolitical boundaries.3 A growing awareness that bioterrorism agents could spread in the same way has raised the level of concern even more. Many practitioners and researchers agree that contact tracing, which is the identification and locating of people who may have been in contact with an infected person, represents an important factor in mitigating the spread of a pandemic.4
Transport networks, whether in the air, at sea, or on land, are continually expanding in terms of distance covered, speed of travel, and the volume of both passengers and goods carried. The increasing use and affordability of passenger air travel has contributed not only to people’s growing mobility, but also to the increased transmission of infectious diseases, such as influenza,5 tuberculosis (TB),6 and SARS,7 as well as a multitude of zoonotic diseases. In addition, the increased awareness of bioterrorism agents and their potential spread via air travel has caused public health agencies (PHAs) to reevaluate the potential spread in flight of these agents.8
According to the World Health Organization (WHO), air transport presents a key challenge to preventing the international spread of health risks.9 In Europe in the 1300s, it took more than 10 years for the deadly Bubonic plaque to spread. Today, a person can travel almost anywhere in the world in a day, and a passenger can carry a fatal strain of avian flu from China to Europe within 24 hours. Indeed, the European Centre for Disease Prevention and Control (ECDC) has stated that air travel was behind the introduction of the influenza A (H1N1) strain into countries that had not been primarily affected previously. Moreover, airlines will likely be a major component when, not if, the next pandemic occurs.
What Is Contact Tracing?
As a means of controlling pandemics, the WHO has laid down guidelines to assist public health agencies in tracing airline passengers. As a background to this process, consider that if a PHA receives a report of a person suffering from an infectious disease, it is the responsibility of the PHA to perform a risk assessment to determine whether any other people are at risk of acquiring the disease due to contact with the infected person and to perform “contact tracing” if needed.
Contact tracing is defined, by the ECDC’s “Risk Assessment Guidance for Infectious Diseases Transmitted on Aircraft” guideline, as “an investigation procedure aimed at acquiring contact information in order to approach contacts that were potentially exposed to pathogens,”10 and by the European Parliament as “measures implemented in order to trace persons who have been exposed to a source of a serious cross-border threat to health, and who are in danger of developing or have developed a disease.”11
The contact tracing of infected or at-risk airline passengers falls under the remit of PHAs that are, in turn, guided by emergency management (EM) practitioners. The current process is that data collection is facilitated by EM practitioners and subsequently collated by PHAs. The EM lifecycle consists of four phases: mitigation, preparedness, response, and recovery. Contact tracing pertains to at least two of those phases: preparedness and response. During the preparedness phase, it is incumbent on PHAs to have the necessary protocols in place to quickly identify an at-risk passenger. Once a threat has been identified, these protocols are acted upon during the response phase.
Information systems, normally complex and multifaceted, have a critical role in EM.12 Such systems consist of multiple stakeholders and require decisions to be made under pressure, in a timely manner, and with valid information.13 To aid this critical role in EM processes, information system tools have been developed to facilitate decision making and are used by emergency responders and decision makers during the phases of the EM lifecycle.14 These tools are paving the way for a digital version of contact tracing to be used as a decision-making tool.
What Can Be Done?
Because of the multifaceted response to an infectious disease outbreak and the possible political, economic, social, and healthcare impacts of an outbreak, it is vital that resources are appropriately allocated, in parallel with the timely dissemination of consistent information.15 The digitization of contact tracing can play a significant role in providing information for identifying and locating passengers at risk from a biological threat, in a timely manner, and using valid data.
In general, PHAs require quick access to passenger data, which means without any significant time delay. The time slot open to initiate and perform contact tracing depends on the incubation period of the specific disease involved and the time left to apply public health measures. For most infectious diseases, the incubation period and the time left to apply such measures is short, further underscoring the need for prompt and accurate contact information. Public health and aviation sectors, together with other stakeholders, must manage public health events in air transport to avoid the international spread of disease.
To assist with contact tracing, WHO developed a ‘’passenger locator form’’ (PLF),16 which currently exists in paper format. The UN’s International Civil Aviation Organization’s “Guidelines for States Concerning the Management of Communicable Disease Posing a Serious Public Health Risk”17 states that the PLF “provides an appropriate method of rapidly collecting passenger contact information: aircraft operators should determine if the PLFs will be kept on board, or at all destination airports. Depending on the specific hazard, the number of PLFs needed may vary, from a few to one for each passenger.” The inference here is that paper copies of the PLF should be kept at airports and on airplanes, to be prepared if and when they are needed. It may be necessary to acquire the data of only a small number of passengers (those in an at-risk area of the airplane), or it may be that the data of all passengers onboard needs to be captured.
In most cases, once a public health threat has been identified, the airline involved would be asked for its passenger manifest, which is collected in a digital format, to aid with the contact tracing of the passengers on that flight. The passenger manifest usually consists of a shortened version of the passenger name record (PNR), and includes the passenger’s name, seat number, and dietary requirements. It can take a few hours to a few days to receive this information, which then needs to be analyzed, leading to a delay in effectively identifying those at risk from a biological threat.
A PNR consists of information provided by passengers and collected by air carriers during reservation and check-in procedures. Noncarrier economic operators, such as travel agencies and tour operators that sell package tours making use of charter flights, also collect and process PNR data. PNR data may include several different types of information, such as travel dates, travel itinerary, ticket information, contact details, baggage information, and payment information. The PNR data is collected for the sole use of the airline, and in many cases lacks vital contact information, including addresses and contact telephone numbers.
In many cases, the only data from PNRs that is of use to public health authorities will be names and nationality information. Many countries do not have the ability to acquire contact information for passengers from passport numbers. Although a telephone number is often requested in the context of the flight booking procedure, this is not a requirement, and the accuracy of the provided information is unknown. It is therefore often problematic to trace passengers using the PNR information alone.
Delays in effective and efficient contact tracing result in the need for a significant increase in resources, such as vaccines and human resources, as EM practitioners must deal with a larger geographical spread (as those potentially exposed continue to travel) and an increase in the number of people potentially exposed. Delays can also result in increased socioeconomic costs, such as increased demand on public health due to retrospective identification of at-risk passengers. In the worst case, delays can potentially result in an increased loss of life.
The quality of the passenger data collected for analysis, from both the PLF and PNR, also poses challenges. More often than not, the data is inaccurate and incomplete, which frequently leads to delays in identification and incomplete tracing of potentially at-risk contacts. Identifying and locating exposed persons through contact tracing is an important procedure during the containment phase of an emerging communicable disease, which forms part of the EM response phase.
Barriers to the identification of at-risk passengers include the current paper-based process, noncollaboration between the airline industry and PHAs, questionable data validity, and privacy laws in multiple jurisdictions. The digitization of this process will allow for an enhanced digital version of contact tracing that will have the capability to be linked to both airline data systems and to public health data systems. Digitization, along with the necessary legislation, should greatly reduce, if not negate, these current barriers.
Where to Now?
PHAs and EM practitioners have indicated that a digital method of contact tracing is preferable to the existing paper-based method (Figure 1 illustrates a prototype digital form). The existing methods (PLF combined with PNR) require greater time to collate and analyze than would a digital version. Thus, locating the “index” passenger (the infected person) on an aircraft, along with the passengers in the “at-risk” vicinity, requires a considerable amount of time and effort from the public health agency. Digitizing contact tracing would provide an appropriate method of rapidly collecting passenger contact information, including:
-
Flight information, including the flight and seat number
-
Personal information
-
Passport information
-
Permanent and temporary address and contact information
-
Emergency contact information
-
Travel companions’ information, both family and non-family
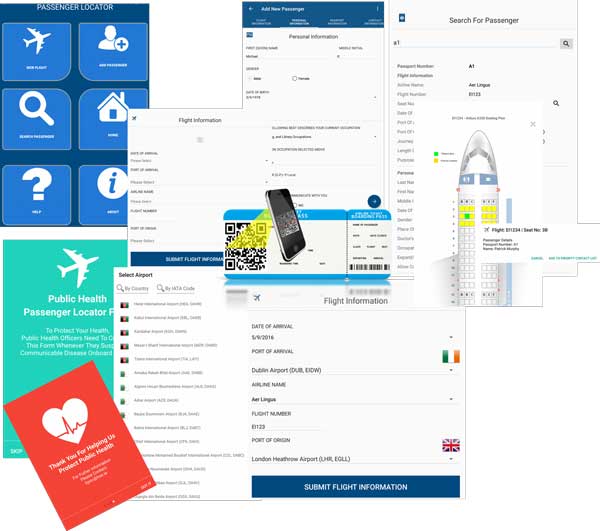
Passengers would fill in a digital form onboard the flight via hand-held devices linked to a database that would auto-populate certain fields of data (collected via the PNR) pertaining to the seat number or boarding card, such as name, home address, contact number, and so on.
EM practitioners and PHAs consider it important to capture additional data, which does not currently form part of the PLF, including:
-
Passenger’s doctor’s name (this information would allow a health practice to be rapidly informed of a potential threat, possibly to be introduced by an existing patient, for passengers local to the port of arrival)
-
Passenger’s occupation
-
Expanded details of the passenger’s occupation (e.g., a person with the occupation of “education” poses a very different contagion risk depending on whether the work environment is independent [a writer or researcher] or is in a school [a primary school teacher has the potential to expose hundreds of children to an infectious disease])
-
Passport issue and expiration dates, which may provide an indication of future travel plans
-
Comment section for PHA members to record details on and tag the recorded passenger
Collaboration between the airline industry, EM personnel, and public health agencies would greatly improve the ability to successfully identify an at-risk airline passenger. A shared, up-to-date digital record of passenger data would almost certainly remove the challenges of collecting and analyzing passenger data. The digital collection makes it easier to verify that each passenger has completed a form and supplied all the information requested. This, in turn, enables digital analysis of the data, which can be carried out quickly and efficiently.
The digital format of the contact tracing system should have the functionality to interact with both airline and PHA systems to enable the collation of passenger information. This cooperation and digitization would certainly require that legislation and agreed service-level agreements be put in place. A European Commission PNR directive has been adopted that obliges airlines to hand EU countries airline passenger data for the prevention, detection, investigation, and prosecution of terrorist offences and serious crime;18 however, it can be argued that this obligatory cooperation could also aid in contact tracing of passengers infected by disease.
Although PNRs currently frequently lack certain passenger data, as discussed earlier, the use of a revised version of the PNR will greatly aid the collection process of passenger data for contact tracing purposes by auto-populating a greater number of fields of data, limiting the time required to collate and locate passengers at risk of exposure and potentially carrying an infectious disease. It is envisaged that digitization would have the capability to auto-populate certain fields of passenger data, via use of the PNR, along with controlling the input of data by the passenger to ensure complete and correct data capture. Digital input can be controlled by limiting the available options to the passenger; for example, not allowing the passenger to input text into a number input or not allowing the passenger to input a return date that is in the past, and by auto-populating certain fields, such as seat number, or by auto-populating an address based on zip code. Uncovering the required data of an at-risk passenger in an efficient manner and without unnecessary use of valuable resources would require such a digitized system.
The digitization of contact tracing, including the involvement of and collaboration with multiple stakeholders, such as the airline industry, EM practitioners, PHAs (through their respective governments), and digital development experts, can provide an effective global framework to prepare for and respond to a biological threat, natural or otherwise, spread via air travel.
References
1“2036 Forecast Reveals Air Passengers Will Nearly Double to 7.8 Billion.” Press release, International Air Transport Association (IATA), No. 55, 24 October 2017.
2Karesh, William B., et al. “Ecology of Zoonoses: Natural and Unnatural Histories.” The Lancet, Vol. 380, No. 9857, 1 December 2012.
3Tatem, Andrew, David Rogers, and Simon Iain Hay. “Global Transport Networks and Infectious Disease Spread.” Advances in Parasitology, Vol. 62, April 2006.
4Smolinsky, Mark S., Margaret A. Hamburg, and Joshua Lederberg (eds.). Microbial Threats to Health: Emergence, Detection, and Response. National Academies Press, 2003.
5Brownstein, John S., Cecily J. Wolfe, and Kenneth D. Mandl. “Empirical Evidence for the Effect of Airline Travel on Inter-Regional Influenza Spread in the United States.” PLOS Medicine, Vol. 3, No. 10, 12 September 2006.
6Flanagan, Paula, Joan O’Donnell, Jolita Mereckiene, and Darina O'Flanagan. “Tuberculosis Contact Investigations Associated with Air Travel in Ireland, September 2011 to November 2014.” Eurosurveillance, Vol. 21, No. 40, 6 October 2016.
7Breugelmans, J. Gabrielle, et al. “SARS Transmission and Commercial Aircraft.” Emerging Infectious Diseases, Vol. 10, No. 8, August 2004.
8Mangili, Alexandra, and Mark Gendreau. “Transmission of Infectious Diseases During Commercial Air Travel.” The Lancet, Vol. 365, No. 9463, 12 March 2005.
9“Management of Events in Air Transport.” World Health Organization (WHO), 2015.
10“Risk Assessment Guidelines for Infectious Diseases Transmitted on Aircraft, Part 1.” European Centre for Disease Prevention and Control, 16 June 2009.
11“DECISION No. 1082/2013/EU of the European Parliament and of the Council of 22 October 2013 on Serious Cross-Border Threats to Health and Repealing Decision No. 2119/98/EC.” Official Journal of the European Union, 11 May 2013.
12Chou, Chen-Huei, Fatemeh Mariam Zahedi, and Huimin Zhao. “Ontology-Based Evaluation of Natural Disaster Management Websites: A Multistakeholder Perspective.” MIS Quarterly, Vol. 38, No. 4, 2014.
13Alexander, David. Principles of Emergency Planning and Management. Oxford University Press, 2002.
14Neville, Karen, Sheila O’Riordan, Andrew Pope, and Mícheál Ó’Lionáird. “Evaluating an Emergency Management Decision Support System with Practitioner-Driven Scenarios: Action Design Research.” In Proceedings of the 2018 International Conference on Information Systems (ICIS), San Francisco, California, USA, 13-16 December 2018.
15Araz, Ozgur M., and Megan Jehn. “Improving Public Health Emergency Preparedness Through Enhanced Decision-Making Environments: A Simulation and Survey-Based Evaluation.” Technological Forecasting and Social Change, Vol. 80, No. 9, November 2013.
16“Strengthening Health Security by Implementing the International Health Regulations: Public Health Passenger Locator Form.” World Health Organizations (WHO), 2005.
17“Guidelines for States Concerning the Management of Communicable Disease Posing a Serious Public Health Risk.” International Civil Aviation Organization (ICAO), 2012.
18“Passenger Name Record.” European Commission, Migration and Home Affairs.



